Wisconsin’s ‘fetal protection’ law forces women into treatment or jail
An investigation by The Marshall Project, The Frontier and AL.com, co-edited and published in partnership with The Washington Post, found that since 1999, more than 50 women have been charged with child neglect or manslaughter after testing positive for drug use following stillbirth or miscarriage.
Since its enactment, Wisconsin’s fetal protection law has weathered two high-profile challenges. Loertscher’s legal team — which included now-Attorney General Josh Kaul — was most successful, securing a federal court ruling that deemed the law unconstitutional. But the win was brief, and due to a technicality, the law remains in effect today.
Loertscher’s case gives the public a glimpse at what can happen at its most extreme. While the law does not require county health officials and hospital workers to report such cases, a 2018 Pew study found Wisconsin practitioners “commonly” misinterpret their legal obligations — something researchers suggest the state should clarify.
War on drugs leads to ‘crack baby’ myth
In 1997, the Wisconsin Supreme Court ruled that a Waukesha juvenile court lacked authority to detain a pregnant woman at a hospital until childbirth on the basis of drug use. Not long after, a bipartisan group of lawmakers gave it that very authority in Act 292, which gave “unborn children” from zygotes to embryos full human rights — the only state to do so.
Bonnie Ladwig, a Republican representative from Racine who introduced the bill, testified: “Cocaine babies and children with fetal alcohol syndrome can be seen as abused children.”
Health professionals warned the fear of punishment would discourage pregnant women from seeking prenatal care and substance use treatment. Some suggested the law would incentivize women to get abortions to avoid detention.
And analysts — and even one of the co-sponsors — doubted its constitutionality. The nonpartisan Wisconsin Legislative Council and Legislative Reference Bureau advised that the liberty and privacy rights enshrined in Roe v. Wade and Planned Parenthood v. Casey would likely outweigh the state’s interest in “unborn human life before fetal viability,” according to the Collaborative for Reproductive Equity at the University of Wisconsin-Madison.
Writing in her book Policing the Womb, the law professor Goodwin said the media used anecdotal reports to fuel a hysteria over so-called “crack babies” — an ostensible “bio-underclass” doomed to lifelong suffering.
The racist crack baby myth cast Black, brown and Indigenous women as bad mothers and their infants as permanently damaged, Goodwin told Wisconsin Watch. She noted that the former director of the National Center on Child Abuse and Neglect claimed — without evidence — that up to 15{a0ae49ae04129c4068d784f4a35ae39a7b56de88307d03cceed9a41caec42547} of African American children would have “permanent brain damage” from gestational cocaine exposure, even though the majority of crack cocaine users are white.
“If this law had the face of middle or upper income white women at the time, it would not have been a law that would have won enactment or support,” Goodwin said.
A longitudinal study has since debunked the myth. Dr. Hallam Hurt, a neonatologist and pediatrics professor at Children’s Hospital of Philadelphia, followed children exposed to cocaine in utero for nearly a quarter of a century.
Hurt found no meaningful differences in development or cognition between the groups with gestational cocaine exposure and without. But both groups — all children from low-income families — performed poorly, leading Hurt and her team to conclude that poverty more powerfully influenced a child’s well-being.
A Wisconsin Watch analysis of DCF data found that today, Wisconsin child protective services disproportionately investigates allegations of unborn child abuse against Indigenous women, compared to their population size. The public defender says she represents a “very high” number of Native American women in Act 292 cases.
‘He is what gave me purpose’
Depression dogged Loertscher since elementary school, but antidepressants exacerbated her suicidal thoughts. She tried to die by overdose several times. A low point came when Loertscher passed out at a bar after drinking. A videotape surfaced showing her unconscious, being raped by multiple men.
That’s when Loertscher began self-medicating with methamphetamine. The stimulant “helped her to get out of bed in the morning,” according to a complaint later filed in federal court. Marijuana also mellowed her symptoms, which her attorneys contend she smoked “fewer than 10 times” that year.
Loertscher’s pregnancy by her then-boyfriend, now husband, compelled her to save her life — and her son’s.
“As soon as I found out that he was going to be a part of us, everything was for him,” Loerstcher said. “He is what gave me purpose.”
She said she disclosed her drug use in hopes of ensuring her son’s health and tried to explain her inability to afford prescription treatment to hospital staff.
“I was trying to self-medicate,” Loertscher said. “They didn’t care. It’s like, they had a certain set of protocols that they had to follow, and it’s like, erase the woman out of the equation.”
‘I don’t matter at all’
Less than 24 hours after Taylor County requested temporary physical custody, a social worker ushered Loertscher into a hospital conference room, where she listened into a court hearing on speakerphone.
On the other line were the court commissioner, corporation counsel, human services staff and another lawyer — court-appointed to represent Loertscher’s fetus. She lacked an attorney.
“It just kind of confirmed the feelings of ‘I don’t matter at all,'” Loertscher recalled.
Pregnant people going through Act 292 proceedings are eligible for state public defenders if they qualify by income. But Sandra Storandt, a social worker with Jackson County, said pregnant women in her county typically lack representation in this initial hearing because it happens so quickly — by law, within 48 hours of filing a request for temporary physical custody.
The authorities wanted Loertscher to remain at the hospital until “medically cleared” and then transferred to a licensed treatment facility. A center in Eau Claire, over an hour from her home in Medford, had availability. In Wisconsin, pregnant women get priority placement in substance use treatment centers.
A court transcript documents the hearing. Asked if she understood the hearing’s purpose, Loertscher said she would not answer questions without an attorney.
The court recessed in a failed attempt to find an attorney to represent her. Loertscher left the conference table and asked to make a call.
“I just followed Tammy down the hallway to her (hospital) room,” the social worker told the court. “She doesn’t want to be part of this.” The commissioner ruled that she had waived her right to participate, noting that they had limited time before they would have to release her.
At this point, authorities had another 24 hours.
A social worker went to Loertscher’s room, holding a phone so she could hear. The county called an obstetrician/gynecologist who claimed Loertscher admitted to knowingly using methamphetamine while pregnant. Prefacing that she was “not an expert witness,” the doctor explained some concerns around methamphetamine use during pregnancy, including low birth weight and possible learning disabilities and inattention to prenatal care.
In 2022, Pregnancy Justice reviewed numerous studies and reports about gestational exposure to various drugs, concluding, “Research tells us that there is no scientific evidence of unique, certain, or irreparable harm for fetuses exposed to cocaine, methamphetamine, opioids, or cannabis in utero.”
The doctor recommended residential treatment; the fetus’ attorney asked the court to force Loertscher into treatment “for this child to have a chance of literally being born.”
Afsha Malik, formerly a research and program associate at Pregnancy Justice, says Wisconsin’s “probable cause” standard means courts need only the “suspicion” of drug use to order commitment. The four other states which permit civil commitment — the Dakotas, Oklahoma and Minnesota — all require “clear and convincing evidence.”
The commissioner found enough evidence to detain Loertscher at the Eau Claire hospital until discharging her to the residential treatment facility.
Separation threatened
After the hearing, Loertscher said the hospital staff warned her she would lose custody of her baby as soon as it was born.
Storandt, the Jackson County social worker, said that in her county, the likelihood of a child staying with a parent is higher than their chance of removal, and separation isn’t always permanent.
But the state public defender practicing in northwestern Wisconsin, who spoke anonymously, said she’s seen newborns taken from parents “many, many times.”
This public defender estimates she handles about one Act 292 case per year. Unlike Loertscher, many of the clients are moms with prior involvement with the child welfare system. Their chief concern: “Am I going to be able to keep my baby after they’re born?”
The attorney said she’s seen foster care requests issued the moment a mom tries to take her infant home from the hospital, “even when I’ve had them make it through treatment, and the babies are born clean, and there’s nothing in their system.”
The conditions required to keep one’s children, or get them back, might appear simple enough: keeping regular contact with a social worker, attending supervised visits, taking parenting classes. But even these may be “unrealistic” for families without reliable transportation, a stable address or a working phone, the public defender said.
“Our system is not built to genuinely help parents, who are indigent, who are drug addicted, who are mentally ill, to actually comply with some of the conditions that counties and states want them to comply with in order to get their kids back a lot of times,” the lawyer said.
Deciding to fight
Loertscher, for the most part, resisted the process.
“I just found out that I was pregnant, and they were threatening to take him away,” she said. “I felt like I had to fight for the both of us.”
Two days after the hearing, Loertscher was supposed to transfer to residential treatment. She refused a blood test required for admission, and instead convinced the hospital to let her go home. She left with prescriptions for her thyroid and depression and plans to see a local nurse practitioner.
The discharge summary noted Loertscher didn’t think she misused substances, and that she “would like to keep the baby and that she would be caring for her pregnancy.”
At the courthouse, Loertscher’s case escalated. Taylor County’s corporation counsel requested to take her into immediate custody, and a judge agreed.
Over the next week, police twice attempted to arrest Loertscher to ensure her presence at court hearings. Loertscher’s family also tried to hire an attorney, but they could not afford the retainer fees.
So on Sept. 4, 2014, Loertscher appeared at her plea hearing without counsel. She disputed the county’s claims that she had committed unborn child abuse, setting the case for trial. If a jury determined her guilty with “reasonable certainty” by “clear, satisfactory and convincing” evidence, the court could detain her for the rest of her pregnancy.
That is, if she ever went to trial. But something else got in the way first. Finding she had violated an earlier court order to go into treatment by refusing the required blood test, the judge sentenced her to comply — or serve 30 days in the Taylor County Jail.
“I can’t have the deputies hog-tie you and take you to that treatment center,” the judge said. “That’s a decision you’ll have to make. But I can punish you if you decide not to obey that order.”
Hauled off to jail
Leaving the hearing, Loertscher reflected on her options: inpatient treatment or jail. Of the two, it was obvious which she’d prefer.
But accepting treatment also meant accepting a diagnosis with which she disagreed. It meant adopting an incorrect label — this time, “addict” — that someone else chose for her.
“They said they were going to put me in treatment and keep me there until I had my child, and then they were going to take him away,” she said. “So that’s where I’m like, ‘Well, I’m just going to have to go to jail then.'”
But jail brought its own risks, including missed prenatal appointments. The jail also refused to provide in-house care until she took a pregnancy test, which she initially refused. According to Loertscher’s eventual complaint, when a guard taunted her about taking a “piss test,” Loertscher lashed out.
She yelled obscenities through the closed door. The guard “grabbed” her by the arm, “tried to pull her out of the cell,” threatened her with a stun gun and then marched her into solitary confinement.
She spent about 36 hours in a “cold and filthy” windowless room with feces on the floor and walls. Her metal bed frame had only a “thin mattress and blanket” at night.
While in solitary, Loertscher says she received another threat. If she didn’t provide a urine sample, she’d remain locked up for the rest of her pregnancy and would have her baby there, which the National Perinatal Association warns is bad for the health of the child and parent.
Eventually, Loertscher found a number for the public defender’s office scrawled on a piece of paper by the phone. She called, and an attorney negotiated her release. She agreed to undergo an alcohol and other drug abuse assessment, comply with recommended treatment and pay for and submit to weekly drug tests, among other things.
After 18 days in jail, Loertscher went home. But she was far from free.
‘Born into chaos’
A week after she left jail, she received a letter from the Taylor County Department of Human Services, saying it had made a separate “administrative finding that she had committed child maltreatment” — a designation separate from her court case and consent decree.
“I had to protect us,” Loertscher recalled, “because what they were doing was so ridiculous.”
So she connected with Pregnancy Justice — then called the National Advocates for Pregnant Women — which teamed up with New York University School of Law and a Madison-area law firm. At the end of 2014, Loertscher filed a lawsuit in federal court, arguing she had been “deprived of liberty and numerous, well-established constitutional rights” after seeking health care.
A month later, during a weekly drug test, her water broke and Loertscher went into labor. At the hospital, she says staff questioned her about Act 292. A police officer stationed outside her room heard the same threat: if she did not cooperate, they would take her baby away.
Said Loertscher: “He was born into chaos.”
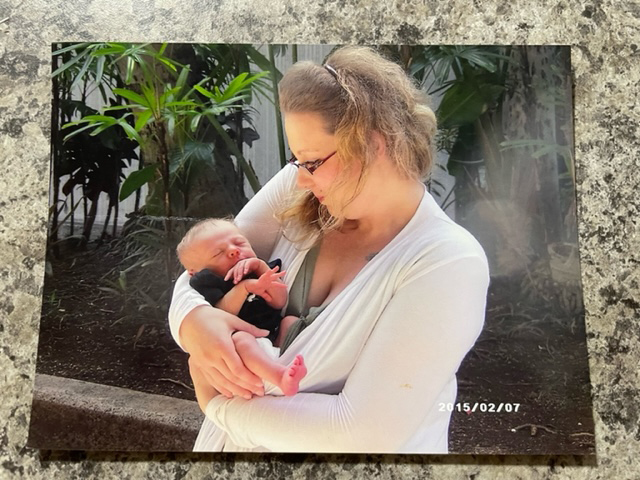
Tamara Loertscher holds her son, Harmonious Ellner, weeks after his birth in 2015. Loertscher was detained and incarcerated in Taylor County during her pregnancy after health officials alleged she was using drugs while pregnant — an allegation she denies. Wisconsin Act 292 allows pregnant people to be detained and forced into treatment if officials suspect drug or alcohol use. (Credit: Courtesy of Tamara Loertscher)
Her attorney raced from Madison to Eau Claire to intervene, but in the end, the hospital allowed Loertscher and her boyfriend to take Harmonious, their newborn, home.
“He is my everything,” Loertscher says. “I just want to make him proud.”
A court win — ‘then they took it away’
Over two years after Harmonious’ birth, the federal court ruled in Loertscher’s favor.
The court found that Act 292 implicated fundamental constitutional rights “to be free from physical restraint” and “coerced medical treatment,” and it was “unconstitutionally vague.”
Each element of unborn child abuse is wide open for interpretation, the judge noted. Its key terms “habitually,” “severe,” even “risk,” are all matters of “degree” that neither the statute nor departmental standards define. As a result, the law could be enforced against any pregnant person with a history of substance use disorder, he said, “regardless of whether she actually used controlled substances while pregnant.”
The state was immediately barred from enforcing Act 292 across Wisconsin.
“I felt like, at least it was for something,” she said. “And then they took that away.”

Dondi Ellner relaxes with his son, Harmonious, shortly after his birth. (Credit: Courtesy of Tamara Loertscher)
Within a week, Republican Attorney General Brad Schimel appealed the decision.
An appeals court panel ruled the injunction was “moot” because Loertscher had left Wisconsin two weeks after Harmonious’ birth, temporarily moving to Hawaii.
“I beat myself up so much,” Loertscher said through tears. “If I would have stayed in that shithole, it (ruling) would have stuck.”
The law remains in effect today.
At least one substantive change to procedure has been made, although it came before Loertscher filed her lawsuit. The Department of Children and Families no longer allows social workers to determine whether or not a pregnant person has committed “maltreatment.” Instead, they only determine whether or not to require “services,” such as counseling or treatment.
“I don’t understand how they can acknowledge that something is unconstitutional, but keep it going,” Loertscher said. “That makes it seem like our constitution doesn’t mean anything to certain people, like, certain people’s rights don’t matter at certain points.”
Wisconsin’s confusing standard
Fetal protection laws place pregnant people into a distinct legal class, says Malik, who at the time she spoke to Wisconsin Watch was with Pregnancy Justice.
While most drug-related offenses relate to possession or distribution, these laws punish pregnant women for use — even if these are legal substances, such as alcohol, which are lawfully obtained.
The behavior identified as unborn child abuse in Wisconsin falls under standards that even those charged with enforcing the law struggle to describe. It requires that a pregnant person “habitually lacks self-control” regarding alcohol or drug use. The habitual lack of self-control must be “exhibited to a severe degree” and create a “substantial risk” that the fetus’ — and eventually, the newborn’s — physical health “will be seriously affected or endangered” unless the parent receives treatment.
When asked by email to clarify what “habitually,” “severe degree” or “serious harm” means, Department of Children and Families communications director Gina Paige said the law “did not include any further language or define these terms.”
Enforcement varies by county. Only Dane, Jackson and Outagamie gave Wisconsin Watch insight into their procedures. Another county provided background information on its approach on the condition of anonymity. A social worker from Jackson provided an on-the-record interview, the others provided answers or statements via email. Officials from Brown and Ashland counties initially expressed interest in speaking but did not follow through with interviews or email responses.
Dane County said it “does not endorse” placing people in a “locked facility to force treatment” and instead favors harm reduction, which it did not define.
‘Being quiet about it isn’t helping anyone’
Seven years after the birth of her healthy baby boy, Loertscher, who now lives in Georgia, is still scarred by her entanglement with Act 292.
“They say that they’re doing it to protect the child, but in reality, at least in my situation, they didn’t care one bit,” she said. “It was all about, for some reason, proving that I was a bad person.”
The detention, incarceration and legal battle has left her with further anxiety and depression. Loertscher has found it difficult to trust anyone outside of her immediate family, leaving her unable to work and even afraid to drive.

Tamara Loertscher and Dondi Ellner are seen with their son, Harmonious. She says of Harmonious: “He is my heart.” (Credit: Courtesy of Tamara Loertscher)
The trauma she and her husband share manifests in overprotective parenting.
But in the last two years, around the time Harmonious began school, Loertscher felt something shift within her: “I finally was like, ‘You know what? I’m not going to let them take all my power away.'”
She started taking better care of herself, socializing more and giving interviews about her experience, because “being quiet about it isn’t helping anyone.”
“What they did didn’t break us, if that was what they were trying to do,” she said. “And our son turned out amazing. He’s smart and he’s happy.”
The 7-year-old is “like a little fish” in the water and loves to read with his mom, and tell her jokes he picked up from books.
His favorite, of late, asks: “What did the alien say to the vegetable garden? Take me to your weeder!”
Loertscher has a message for anyone else caught up in Wisconsin’s fetal protection law.
“I want to tell them that they can be brave,” she said. “They can come forward and they can say that what happened to them is wrong, because it was.”
What to do if you are pregnant and struggling with substance use in Wisconsin
There is currently no directory of Wisconsin-based doctors and midwives experienced in providing care to pregnant people with substance use disorder, says Dr. Charles Schauberger, who is board certified in both obstetrics and addiction medicine and has dedicated the past 10 years of his career to caring for pregnant women with substance use disorder.
Enforcement of Act 292 varies depending on the county where one resides. But Schauberger’s experience tells him that “if a care team has the reputation of working hard to keep patients in treatment and providing great prenatal care, county health authorities, including CPS, are much more likely to back off.”
Schauberger offered this advice for pregnant people with substance use disorders:
- Begin prenatal care as soon as possible. This will be safer for you and your baby.
- Don’t delay treatment or attempt to hide your pregnancy.
- Be selective about whom you see for prenatal care, seeking out medical providers experienced in caring for women with substance use during pregnancy. Drug treatment programs and other women who have used drugs and had recent pregnancies may be good sources for referral.
Pregnancy Justice has created a fact sheet for healthcare providers and pregnant people, and offers this advice in a know your rights sheet:
- Consider speaking to an attorney or visiting the group’s birth rights guide (English and Spanish) before disclosing past drug use to your doctor.
- Contact Pregnancy Justice at 212-255-9252 or through their website if you are accused under Act 292 and need free legal advice.
If you or someone you know is struggling or in crisis, help is available 24/7. Call or text 988 to reach the 988 Suicide & Crisis Lifeline, or use the chat feature at 988lifeline.org.
The nonprofit Wisconsin Watch collaborates with WPR, Milwaukee Neighborhood News Service, PBS Wisconsin, other news media and the University of Wisconsin-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by Wisconsin Watch do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.
